The vaccine
Why a nasal vaccine?
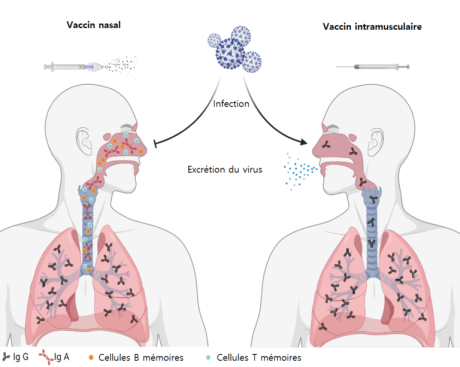
Natural infection with SARS-CoV2 induces a mucosal and systemic immune response. For example, the mucosal immune response is characterized by the presence of immunoglobulin A (IgA). Similarly, the systemic immune response is characterized by the presence of immunoglobulin G (IgG). In other words, IgA are actively involved in the protection of the upper respiratory tract, whereas IgG mainly protect the lower respiratory tract.
In fact, vaccines that are administered intramuscularly or intradermally induce primarily IgG, not IgA.
So, most currently available vaccines induce sufficient immunity to protect against severe forms of the disease. But, they are not necessarily sufficient to achieve sterilizing immunity.
On the contrary, a vaccine administered by the nasal route allows the induction of a protective systemic response but also of a local response in the nasal mucosa. So, it blocks the natural entry point of the virus. Consequently, it enables the transmission chain to be stopped.
An innovative vaccine more adapted to the variability of the virus
The currently available vaccines are all based solely on the SARS-CoV2 Spike protein. Indeed, it shows a rapid ability to mutate and potentially reduce the effectiveness of the immune response induced by vaccination.
Furthermore, the analysis of the work carried out by several research teams on SARS-CoV1 and MERS has allowed us to identify, in addition to its Spike protein, other parts of the virus not subject to mutation. Of course, these parts are able to contribute to the induction of a protective immune response in preclinical models.
Thus, our candidate vaccine benefits from a broader valence, potentially able to cope with the appearance of new variants.
Finally, its adjuvant-free formulation gives it great stability, making it possible to bypass the cold chain. In conclusion, this would facilitate vaccination, particularly in developing countries.